

However, the relationship between sudden changes in MELD score immediately prior to LT surgery and outcomes was not examined. demonstrated that patients with a rise in MELD score of >10 over their time on the waitlist tended to experience worse 1-, 3-, and 5-year post-LT survival 11, which was later replicated in a large Eurotransplant registry analysis 12. In a single center analysis, Gyori et al. Another study analyzing 69,643 waitlist registrants found that a rise in MELD score of >30% during a seven-day period was associated with an increase in waitlist mortality but lacked association with post-LT mortality 16. in 2004 reported that a preoperative rise in MELD score of ≥5 within 30 days of liver transplantation was not predictive of post-LT survival 14. Using the Organ Procurement Transplant Network/United Network for Organ Sharing (OPTN/UNOS) registry, Northup et al. ACLF often impacts the Model for End-Stage Liver Disease (MELD) score, a validated objective predictor for early pre-LT mortality and the primary allocation criteria for liver transplantation in the United States (US) 6, 7, 8.Īlthough a ≥5 points rise in MELD score over 30 days in the setting of ACLF has been shown to predict pre-LT waitlist mortality 9, 10, the data are conflicting in terms of post-LT survival, in part due to widely varying time frames that have been evaluated 9, 11, 12, 13, 14, 15. In patients with liver failure in the setting of cirrhosis, acute-on-chronic liver failure (ACLF) is a clinical entity characterized by sudden onset and rapid progression of underlying hepatic dysfunction which may be accompanied by multi-system organ failure with high risk of short-term mortality (50–90%) without prompt supportive measures and liver transplant (LT) surgery 1, 2, 3, 4, 5.
The increased risk of pre-LT mortality associated with severity of clinical decompensation assessed by the magnitude of pre-operative D-MELD persists in the early post-LT period. Moreover, pre-operative D-MELD > 10 was associated with nearly a two-fold increased risk for 30-day post-LT mortality (adjusted HR, 1.89, 95% CI: 1.30–2.77) compared to D-MELD 0–4. One-point incremental increase in pre-operative D-MELD (adjusted HR, 1.07, 95% CI: 1.04–1.10) was associated with higher 30-day post-LT mortality. Impact of D-MELD as a continuous and categorical variable (D-MELD 0–4, 5–10, >10) on early, 30-day post-LT mortality was assessed. Delta-MELD (D-MELD) was defined as recipient MELD score at LT minus lowest MELD score within the preceding 30 days.
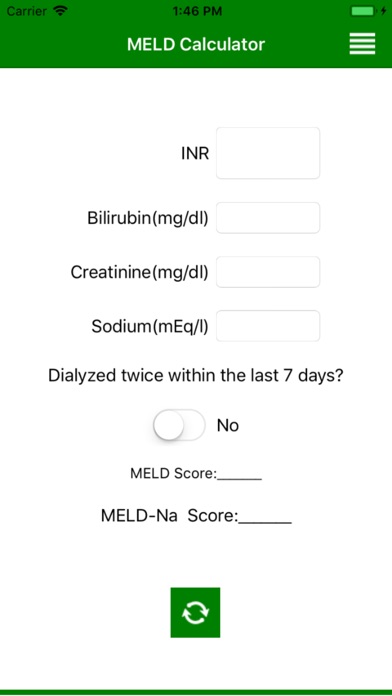
MELD SCORE SERIAL
Using the serial Model for End-Stage Liver Disease (MELD) scores recorded in the United Network for Organ Sharing national registry (2010–2017), we analyzed post-LT mortality among adult LT recipients based on the degree of fluctuation in MELD score during the 30-day period prior to LT surgery. Clinical decompensation immediately prior to liver transplantation may affect post-liver transplant (LT) outcomes.


 0 kommentar(er)
0 kommentar(er)
